Flow can be defined as uninterrupted motion like a river or a freeway.
Now think of all the patient journeys commencing from pre-hospital to triage, through the Emergency Department and either back to the community or to the ward and then back to the community. Now think of all these patient journeys happening all at once every day – that is patient flow.
What happens when the flow gets clogged up?
At a basic level, overcrowding is when there is no space or no staff to see the next patient.
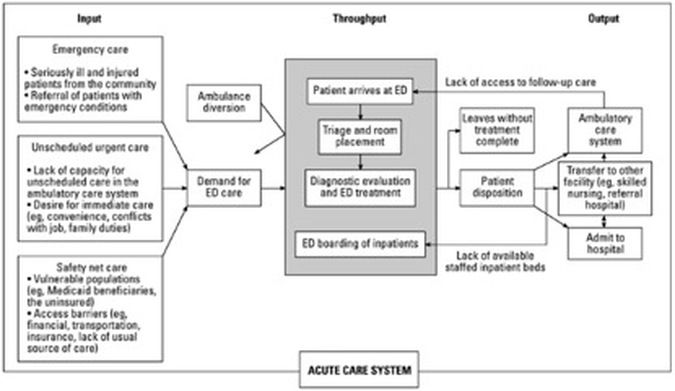
Inputs;
- more patients
- more older patients
Throughputs;
- Any inefficiencies re assessing patients or getting pathology/imaging done
- Time taken for specialist teams to review and admit patients
- Time taken to get the patient upstairs – any inefficiencies in bed management.
- Not enough staff or staff not matched to patient volume
- Physical design problems
Outputs;
- Access Block: “The situation where patients who have been admitted and need a bed have been delayed (usually measured as more than 8 hours) from leaving the ED because of lack of inpatient bed capacity.”
- Lack of community services including; primary care, case management for patients with chronic disease, outpatient clinic appointments.
- What are the consequences of ED overcrowding?
- Nearly everything bad you can think of; increased mortality, increased morbidity, increased overall length of stay, increased errors, greater time to antibiotics, greater time to reperfusion, more missed MIs, worse patient satisfaction, more did not waits.
A quick example.
After the formation of a NEAT taskforce including senior medical and nursing managers as well as a data analyst, within one year, implementing 25 different reforms with regular updates back to the rest of the hospital, they improved from 32% patients seen and discharged within 4 hours to 62%. Their mortality decreased from 2.3% to 1.7%.


 RSS Feed
RSS Feed
