Terminology
Clinical Terminology
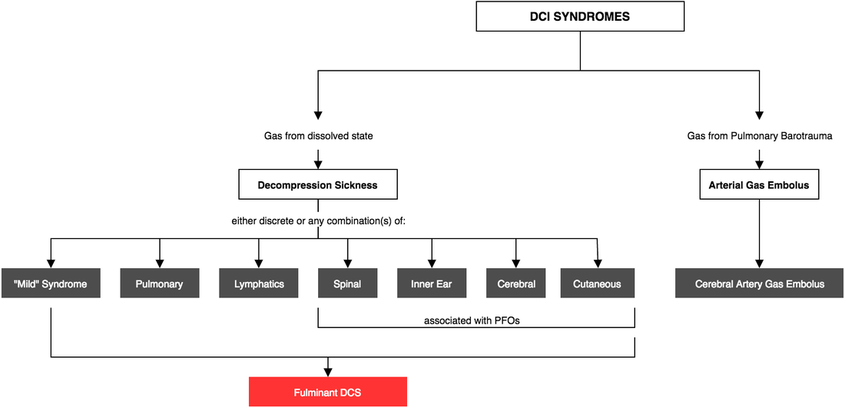
Rule 1. Call everything decompression related "Decompression Illness (DCI)"
Rule 2. Use evolution of symptoms and organ involvement to describe the type of DCI"
The Disclaimer
DCI, DCS, AGE are all academic terms - useful in research to understand pathophysiology and test biologically plausible treatments and have limited use when describing cases in a clinical setting (see above).
Rule 1. Call everything decompression related "Decompression Illness (DCI)"
Rule 2. Use evolution of symptoms and organ involvement to describe the type of DCI"
- Evolution: Progressive, Remitting, Static, Relapsing
- Organs: Musculoskeletal, Neurological, Constitutional, Cutaneous
The Disclaimer
DCI, DCS, AGE are all academic terms - useful in research to understand pathophysiology and test biologically plausible treatments and have limited use when describing cases in a clinical setting (see above).
- Decompression Illness (DCI) = all encompassing pathology arising from decompression
- Decompression Sickness (DCS) = Pathology from bubbles from dissolved state, be it in blood or tissues
- Cerebral Arterial Gas Embolism (CAGE) = Pathology from bubbles from lung barotrauma, specifically, going to the brain
- Venous bubbles going through a PFO have a different clinical presentation to CAGE (cerebral gas embolism)
- Although the term AGE exists - cerebral is the only well documented and researched entity. Other forms of AGE such as inner ear and spinal are usually a combination
DCS Pathophysiology
DCS
Step One: Making Bubbles
Step Two: Bubbles Causing Trouble
CAGE
Step One: Making Bubbles
Step Two: Bubbles Causing Trouble
Step One: Making Bubbles
- Relies on gas (usually N2) being supersaturated in the body - which occurs when the body is compressed (Henry's Law)
- Longer/deeper compression = more N2 in the blood/tissues
- As the pressure decreases, N2 comes out of blood & tissues thus forming bubbles
Step Two: Bubbles Causing Trouble
- Bubbles in the venous system can cause embolic phenomena (including passing through a PFO)
- Bubbles can irritate endothelium causing vasoconstriction, endothelial damage, release of complement (which makes more bubbles) and capillary leak (ie less blood - and O2 - to the mitochondria
- Maximal bubbles in the venous system occur at 30-60min - usually when symptoms start to become apparent
CAGE
Step One: Making Bubbles
- Bubbles FROM the arterial system (as opposed to IN the arterial system, as can happen with venous bubbles going through a PFO) are formed by Pulmonary Barotrauma
Step Two: Bubbles Causing Trouble
- Bubbles are typically larger than DCS bubbles, causing an acute onset in symptoms (typically on reaching the surface), profound (eg loss of consciousness) and phasic (see below)
Syndromes
Combination & Fulminant Disease
- Mild syndrome occurs most commonly in combination, but any permutation of the DCS's can occur - so don't stop looking when you find 1 or 2 or 3...
- Other combinations include: pulmonary + spinal, cutis marmorata + spinal & 'mild' syndrome rash + lymphatics
- Fulminant DCS implies the badder end of the spectrum, most commonly from pulmonary DCS
"Mild" Syndrome
- The reason for this category was to establish symptom(s) that would benefit from hyperbaric therapy but could be withheld if the logistics (including cost) was considered not to outweigh the benefits of therapy
- With hyperbaric therapy these divers recover faster
Includes:
- Musculoskeletal pain: deep boring ache, proximal joint pains, onset variable (often early)
- Constitutional: fatigue worse than expected, malaise
- Subjective sensory changes: non dermatomal, can migrate or be phasic and no evidence of loss of power
- Rash: fine & erythematous, commonly on the trunk and less confluent than cutis marmorata
Pulmonary DCS (The 'Chokes')
- Can occur either as a large air embolus straining the right heart like a "Gas PE" or a 'shower' of small emboli, exacting the same strain
- Can progress to "cardiopulmonary DCS" - which is essentially fulminant DCS
- Onset often occurs < 30 min
- Rarely occurs as an isolated DCS
Cutaneous DCS (Cutis Marmorata)
- Associated with PFOs and CAGE (alone, causes no risk)
- Described as "pinkish-blue" marbled rash
- Onset < 1 hr
- See 'mild syndrome' (above for the other type of DCS rash)
Spinal DCS
- Normally early onset
- Classical symptoms include bilateral sensory and motor changes
- Can also present as pain in the shoulder, hips, back or abdomen
- Cause of spinal DCS thought to be tri-fold
- Bubbles dissolved in white matter and now coming out of tissue
- Bubbles crossing a PFO (since spinal DCS is associated with PFOs) and growing and causing ischaemia/infarction
- Bubbles in epidural veins encouraging venous stasis and clotting (least amendable to hyperbaric therapy)
- Bubbles dissolved in white matter and now coming out of tissue
Inner Ear DCS
- Associated with dives > 30m
- Vestibular symptoms are greater than cochlear symptoms
- Has a variable response to hyperbaric therapy
Cerebral DCS
- Unlike CAGE, is thought to be due to small bubbles from dissolved state (typically from tissues and venous blood), crossing PFO into arterial system spreading throughout the cerebral vasculature, causing a cascade:
- Small bubbles 'squeeze' through smallest cerebral arteries/arterioles
- Mechanical stress results from this
- An inflammatory response occurs to the mechanical stress
- Global vessel narrowing causes a cumulative decreased state of perfusion
- Patient symptoms reflected as 'dysexecutive symptoms' rather than stroke-like symptoms (as is seen in CAGE)
- As a result of these sometimes 'non-specific' symptoms, this can be picked up late, but is thought to occur early
Lymphatic DCS
- Often presents with patchy oedema +/- rash
CAGE
- Due to barotrauma from uncontrolled ascend (but often no historical or clinical evidence of this!)
- Symptoms are sudden onset
- The suggested mechanism is due to a large air embolus causing a large area of cerebral ischaemia - thus the "stroke-like symptoms"
- Often transient as bubble(s) redistribute - thus the phasic nature
- Further exertion can cause more bubbles to embolise