| Viet Tran Pre-hospital cardiac arrest from a limb laceration; let's take a journey that lacks evidence, is full of controversy and where right answers (and the trauma room) are always shades of red. It was the perfect night shift. 5am. The home stretch. The well rested medical registrar finishes admitting the only patient referred in the last 6hrs and exits with a thoughtful observation, “It’s been a quiet night for once”. Cue the "Bat-phone" |
What's Her Prognosis?
To start with, she has a 100% chance of sustained death if we don't do anything. That is, if we don't do anything to an otherwise healthy, young female with a reversible cause, albeit without a robust "chain of survival".
The current literature suggests that "survival to discharge" is anywhere between 0-17% (1), with the biggest study in this series showing a 7.5% chance of survival (2). Note that we have not touched on the morbidity of such patients, but traumatic arrests who survive tend to do better neurologically than medical cardiac arrests. A systematic review of Out of Hospital Traumatic Cardiac Arrest shows that of the survivors (3):
- 40% had a good neurological outcome
- 20% had moderate disability
- 30% had severe disability
- 10% were vegetative
- Children had worse neurological outcomes vs adults
As a comparison, the "survival to discharge" of medical out of hospital arrests is about 10% (4,5) and in hospital arrests around 24% (6)
1. Soar, Jasmeet et al. "European Resuscitation Council Guidelines For Resuscitation 2010 Section 8. Cardiac Arrest In Special Circumstances: Electrolyte Abnormalities, Poisoning, Drowning, Accidental Hypothermia, Hyperthermia, Asthma, Anaphylaxis, Cardiac Surgery, Trauma, Pregnancy, Electrocution". Resuscitation 81.10 (2010): 1400-1433.
2. Lockey, David, Kate Crewdson, and Gareth Davies. "Traumatic Cardiac Arrest: Who Are The Survivors?". Annals of Emergency Medicine 48.3 (2006): 240-244.
3. Zwingmann, Jörn et al. "Survival And Neurologic Outcome After Traumatic Out-Of-Hospital Cardiopulmonary Arrest In A Pediatric And Adult Population: A Systematic Review". Critical Care16.4 (2012): R117.
4. Nehme, Ziad et al. "Population Density Predicts Outcome From Out-Of-Hospital Cardiac Arrest In Victoria, Australia". Med J Aust 200.8 (2014): 471-475.
5. Finn, Judith et al. "Relative Survival Of Out-Of-Hospital Cardiac Arrest Patients In Perth, Western Australia". Resuscitation 83 (2012): e5.
6. Go, A. S. et al. "Heart Disease And Stroke Statistics--2013 Update: A Report From The American Heart Association". Circulation 127.1 (2012): e6-e245.
Back to the issue at hand: How are we going to prepare for this patient?
By failing to prepare, you are preparing to fail
- benjamin franklin
Follow the mantra “place, people, equipment, drugs”
| Place Your best stocked resus bay (or trauma bay if you have one) - most hospital will have a preferred resus bay Don't forget to get the rest of your department in order People Remember it's night, so less Chef's in the kitchen, which can work both in your favour but also against. Seek out people in the hospital:
Equipment Airway including difficult airway kit, ventilator/BVM, fluid warmers, rapid infusers, interosseous, central and arterial line equipment, OG tube, IVC equipment, tourniquet or other haemeostatic devices, thoracotomy kit (not opened), scalpels and drains to formalise finger thoracotomies, warming blanket. Drugs O-ve, O-ve, O-ve, O-ve, start thawing FFPx2u (or as per local MTP), RSI drugs, sedation maintenance, TXA, Ca, Adrenaline, more blood products |
Most trauma centres will have an “autopilot” mechanism that works like a code blue or code STEMI to action most of the above personnel. Be familiar with who and what they will and will not action - time is of the essence.
Just What Is A Massive Transfusion Protocol (MTP) All About?
The timely requisition of blood to replace blood, as simple as it sounds, has only emerged as a 'best practice' within the last 2 decades. The idea being;
- If you're losing blood, replace it with blood
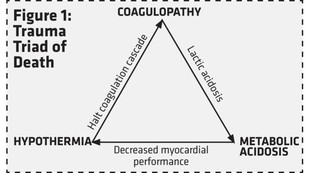
- Up to 25% of Trauma patients requiring MTP will develop traumatic coagulopathy (1), so replace what they're deplete of
- Crystalloid, although expanding the intravascular volume, has no oxygen carrying capacity and makes the coagulopathy worse, so dont.
Who needs it?
Gestalt has always played a big role in it's activation. For those that lack such gestalt (or to confirm it) the “ABC score for massive transfusion” can be used as a guide (it has been validated)(2,3). Remember, it's not a guide to “give blood” but one to give it via an MTP.
How do we give it?
"Like for like" is the theory - initially at least. So this means; Packed cells:FFP:Platelets = 1:1:1
To make it complicated, platelets are often “pooled” into 4 units per pool.
Therefore, some MTPs cycle between 2 packs:
- Pack 1: 1u plt, 2u PRBC, 2u FFP
- Pack 2: 2u PRBC, 2u FFP, no plt
What about the other stuff?
TXA seems to be thrown around quite a bit since the CRASH-2 trial (4). Well worth a read to come to your own conclusions. Bottom line is mortality benefit within the first 3 hrs, thereafter there's thromboembolic risks.
Cryo, Ca, FVIIa; Cryo seems to be favoured over FFP in europe, Ca is worth giving if deficient and FVIIa should be guided by the haematologist ie not a first or second or third line agent.
ROTEM is also coming into vogue as a point of care device that gets to the bottom line - basically works out how good a clot is in terms of time to formation and size and directs towards which blood products and factors would help reverse the traumatic coagulopathy the best. It's a little beyond the breadth of this (5).
1. Holcomb, John B. et al. "Transfusion Of Plasma, Platelets, And Red Blood Cells In A 1:1:1 Vs A 1:1:2 Ratio And Mortality In Patients With Severe Trauma". JAMA 313.5 (2015): 471.
2. Nunez, Timothy C. et al. "Early Prediction Of Massive Transfusion In Trauma: Simple As ABC (Assessment Of Blood Consumption)?". The Journal of Trauma: Injury, Infection, and Critical Care 66.2 (2009): 346-352.
3. Cotton, Bryan A. et al. "Multicenter Validation Of A Simplified Score To Predict Massive Transfusion In Trauma". The Journal of Trauma: Injury, Infection, and Critical Care 69.Supplement (2010): S33-S39.
4. Effects Of Tranexamic Acid On Death, Vascular Occlusive Events, And Blood Transfusion In Trauma Patients With Significant Haemorrhage (CRASH-2): A Randomised, Placebo-Controlled Trial". The Lancet 376.9734 (2010): 23-32.
5. Da Luz, Luis Teodoro et al. "Effect Of Thromboelastography (TEG®) And Rotational Thromboelastometry (ROTEM®) On Diagnosis Of Coagulopathy, Transfusion Guidance And Mortality In Trauma: Descriptive Systematic Review". Critical Care 18.5 (2014): n. pag.
Here she comes...
How do you 'run' a Traumatic Cardiac Arrest?
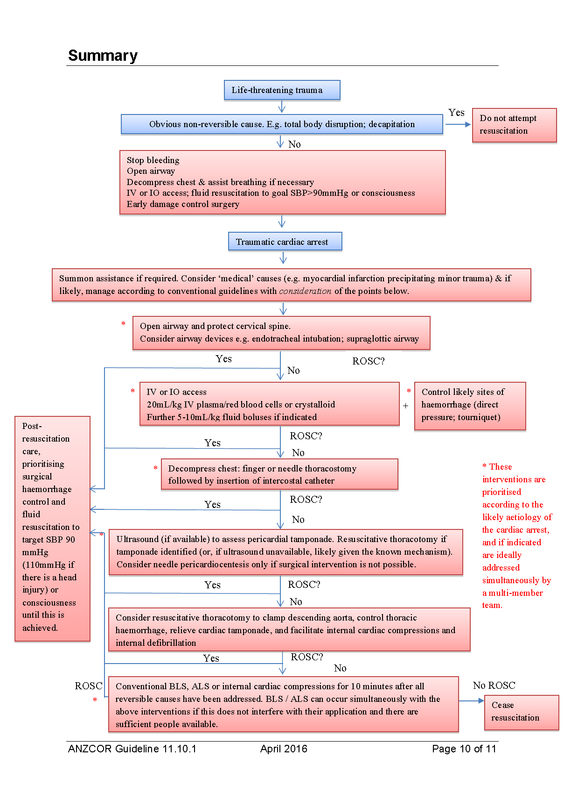
| It essentially boils down to 5 things:
b. Stop blood coming out; wound haemostasis, correct clotting, REBOA, correct the "lethal triad" c. Stop blood going into the wrong places; bilateral finger thoracotomies, thorocotomy (needle paracentesis is second line), aortic clamp d. Make blood go round and round; thoracotomy, internal cardiac massage/defibrillation |
Lets Apply This To The Patient
Whilst CPR is happening, the patient is intubated using video laryngoscopy on first attempt and ventilation is by BVM whilst CPR is occurring.
Circulation
1. Get Blood In
Given the lack of blood in her vascular system, IV access is difficult and we resort to 3xIOs. The O -ve is running simultaneously through 2 of them and 2 more units are to follow (and activation of the MTP).
2. Stop Blood Coming Out
The wound (assumed to be the cause of hemorrhagic shock and arrest) is not bleeding (probably because there's no more blood to lose), and a BP cuff is applied and inflated to 300 mmHg just in case. Coagulation profile has been sent and FFP is being thawed. REBOA might also be an option if damage control surgery is delayed, or in the prehospital setting.
3. Stop Blood Going Into The Wrong Place
FAST scan was performed and showed no blood in the pericardium, no PTX, no blood in the abdomen.
4. Make The Blood Go Round and Round
The decision to proceed to thoracotomy and to do internal massage/defib and clamp the aorta is decided against given haemeostatic control of the underlying cause. External CPR continues.
About that fast scan...this is what the cardiac view looked like:
Uh oh. Cardiac Standstill
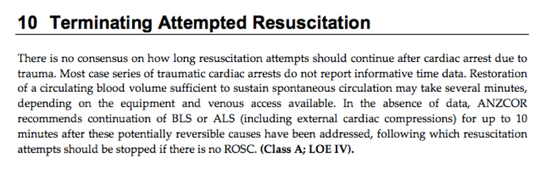
Like most things in trauma, there is little literature, and those that do exist, consider that “survival to hospital admission” approached “100%” for those patients with cardiac standstill on initial bedside echo (1). Unfortunately POCUS is still an emerging utility in emergency medicine and cardiac standstill on eFAST in a traumatic arrest patient has not been acknowledged in the guidelines.
For comparison, cardiac standstill in non-traumatic arrest has a 0.9% rate of survival to discharge (2).
1. Cureton, Elizabeth L. et al. "QS243. The Heart Of The Matter: Utility Of Ultrasound Of Cardiac Activity During Traumatic Arrest". Journal of Surgical Research 144.2 (2008): 363-364.
2. Blaivas, Michael and John Christian Fox. "Outcome In Cardiac Arrest Patients Found To Have Cardiac Standstill On The Bedside Emergency Department Echocardiogram". Acad Emergency Med 8.6 (2001): 616-621.
Ceiling of Care?
We’ve addressed the latter, so we decide to fulfill the former by filling her up with 4 units of O -ve, continue external CPR and make a decision on termination of our attempt at resuscitation depending on what we find following the 4 units.
Time to do a pulse check and echo
As the anaesthetic team wheel the patient out, you notice the sunlight coming through the one window in your emergency department. You look at the triage screen and have a sigh of relief that the department is still under control.


 RSS Feed
RSS Feed
