- Incidence
- Biomarkers
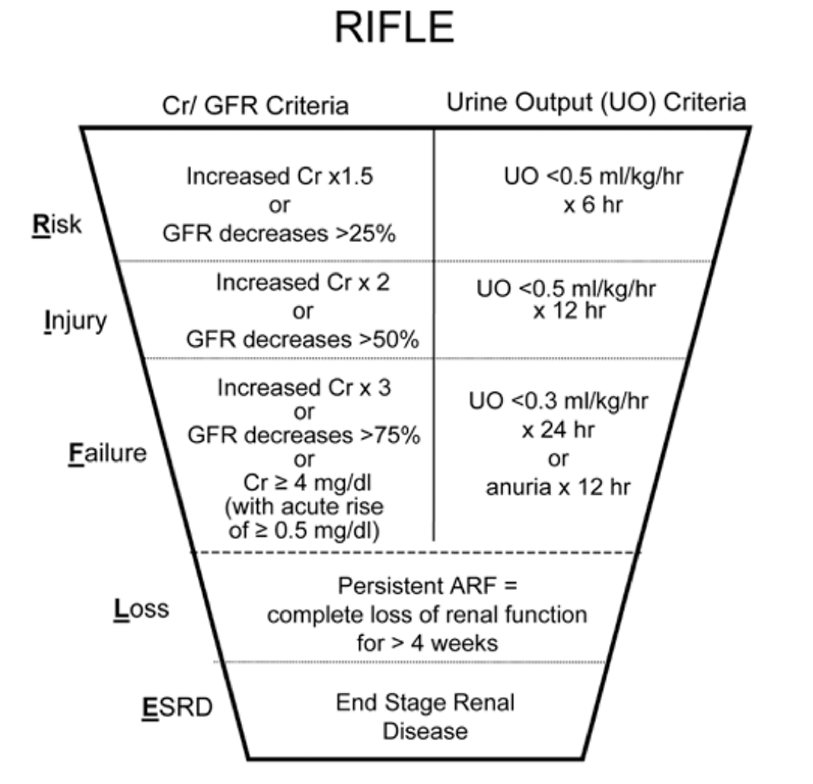
- Classification
- Management
| Admissions
| Acute kidney injury (AKI) is a big deal. Up to 20% of hospital admission have it, and up to 36% of those who have it die. It's an even bigger deal when they're critically ill - up to 60% who develop AKI will die. Yes, i hear you..."22-67% of ICU admissions, that's such a wide variation its meaningless!" Read on and find out the meaning behind such meaningless. |
| Definition ˈbʌɪəʊmɑːkə(r)/ Noun “…a broad subcategory of medical signs – that is, objective indications of medical state observed from outside the patient – which can be measured accurately and reproducibly.” | Biomarker Quality Wish List (what you want in your biomarker)
|
| Urine Output Although not classically seen as a biomarker, it has its benefits in being universally available (you've got your answer if it isn't), familiar and for the most part, clinically relevant. Of course it can be invasive to monitor, non-specific, nor sensitive and most importantly, a late sign. Serum Creatinine Another stalwart of kidney disease and an essential marker in the chronic kidney disease armoury. With acute kidney problems it still suffers from the same stuff as urine output, most notably the lateness of its change. Creatinine Clearance The creatinine is key to its calculation, compounded by the subjective nature of calculating body surface area (does anyone else have trouble estimating height and weight...or is it just me?). Oh, and GFR is untested in the acute state as it really assumes a steady state GFR. Serum Urea Again, a later marker of kidney injury but holds its own as a marker for severity, as in, "His urea is 50 mg/dL...he needs to be dialysed". Novel Renal Biomarker This is the dream. The "Troponin" of the kidney. There's research out there, nothing worthy of validating in the literature just yet. Some of the candidates include:
“Clinical appraisal of a patient using standard parameters such as serum Creatinine and Diuresis remains the cornerstone for now” Lameire N, Vanholder R, Van Biesen W. How to use biomarkers efficiently in acute kidney injury. Kidney International. 2011;79(10):1047-1050. |
Honore P, Jacobs R, Joannes-Boyau O, Verfaillie L, De Regt J, Van Gorp V et al. Biomarkers for early diagnosis of AKI in the ICU: ready for prime time use at the bedside?. Ann Intensive Care. 2012;2(1):24.
Bellomo R, Kellum JA, Ronco C: Defining acute renal failure: physiological principles. Intensive Care Med 2004, 30:33–37.
Devarajan P: Emerging biomarkers of acute kidney injury. Contrib Nephrol 2007, 156:203–212
Lameire N, Vanholder R, Van Biesen W. How to use biomarkers efficiently in acute kidney injury. Kidney International. 2011;79(10):1047-1050.
| The picture to the left is pretty self explanatory. Some rules and recommendations for RIFLE:
Of course, with any first edition there were caveats;
|
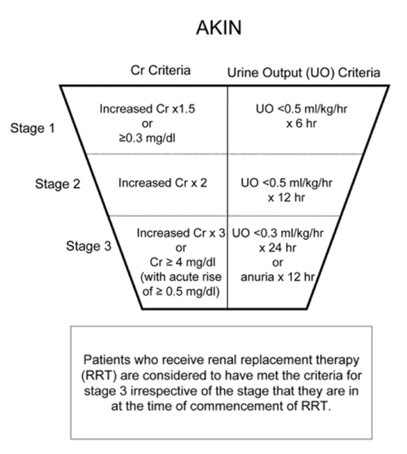
The main difference to RIFLE include
- Dropping "Loss" and "ESRD" (after all, there's nothing acute about them)
- Dropping "GFR"
- Changing R, I, F to Stage 1-3 and calling the whole thing "Acute Kidney Injury"
- Automatically making acute dialysis Stage 3 AKI
- Validation studies for RIFLE revealed that many patients not meeting criteria had poor outcomes with Crea > 0.3 mg/dL - so this was included in AKIN
| The picture to the left is pretty self explanatory. Some rules and recommendations for AKIN:
Of course, with any second edition there were caveats;
|
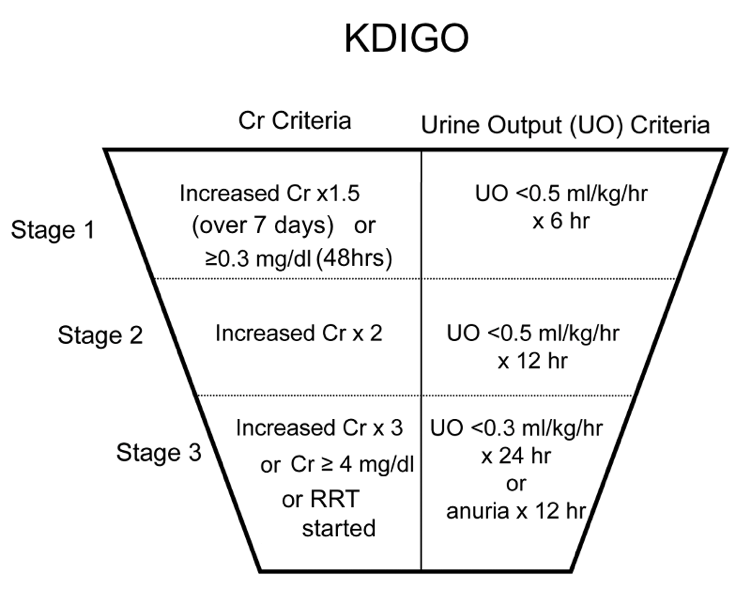
- Dropped the stage 3 classification of Crea > 0.5 mg/dL
- Increased the time frame for creatinine rise from 48 hrs to 1 week
| The picture to the left is pretty self explanatory. No, it really is. Caveats are pending, awaiting validation studies to poke holes in it. DID YOU KNOW KDIGO have a FREE app (android and iphone) with guidelines and recommendations on everything "acute kidney". Get it while its hot (click on the buttons below) |
From experience, most people use KDIGO, thinking that they're using RIFLE.
Who will challenge the KDIGO clan and come up with the 4th revision of the AKI classification? What will their acronym be? Only time will tell.
Kellum JA, Levin N, Bouman C, Lameire N (2002) Developing a consensus classification system for acute renal failure. Curr Opin Crit Care 8(6):509–514
| Hoste E, Bagshaw S, Bellomo R, Cely C, Colman R, Cruz D et al. Epidemiology of acute kidney injury in critically ill patients: the multinational AKI-EPI study. Intensive Care Med. 2015;41(8):1411-1423. Click on the paper to access the PubMed view (it's not free, so you your institutional access if you have one). | By the numbers:
Mortality according to stage
(ie 7x as likely to die if you're stage 3) |
| Our friends Hoste et al from the epidemiolgy paper (the best one out there thus far) found that out of 666 patients, the cause of their AKI was; |
| From this list you can see that n=117 or 17.6% of AKI is caused by renal problems, but the overwhelming majority is pre-renal. Hoste E, Bagshaw S, Bellomo R, Cely C, Colman R, Cruz D et al. Epidemiology of acute kidney injury in critically ill patients: the multinational AKI-EPI study. Intensive Care Med. 2015;41(8):1411-1423. |
| 1. Pre-renal Treat the sepsis, treat the hypovolemia, treat the pump ie perfuse the kidneys. Diuretics have a theoretical role of reducing energy expenditure within the nephron thereby requiring a lower rate of oxygen supply...we'll talk more about this later. 2. Renal Stop the drugs and treat the HRS 3. Post-renal Fix the obstruction. Importantly, an acute rise in Crea is not uncommon in post renal AKI (only so much will accumulate in the bladder, the rest will stay in the plasma...much like K). Despite such impressive creatinine rises, the fall is equally as fast once the obstruction is relieved (assuming its timely). Anecdotally a post renal obstruction Crea of 0.8mg/dL normalised within 24hrs without requiring dialysis! Diuretics in Renal Failure Diuretics are theoretically good for the kidneys because:
The Evidence
The Final Word on Diuretics in AKI “Diuretics should not be used to prevent or treat AKI, except in the management of volume overload” Recommendation by The European Society of Intensive Care Medicine and the Kidney Disease Improving Global Outcomes (KDIGO) |
| “Little variation in AKI occurrence & mortality among levels of health care” |
- AKI - it's a (common, serious) thing
- Diagnosis: RIFLE/KDIGO ie crea or UO (and use the same language)
- Diuretics for overload - dont overthink it
- The kidneys are still a mystery!



 RSS Feed
RSS Feed
