| Viet Tran Ever had that patient with haematemesis that you thought..."they're probably well enough to go home"? Or perhaps stopped and thought "What's the deal with omeprazole in upper GI bleeding (UGIB)"? Today we'll go from one end of the spectrum with clinical decision rules (CDR) in UGIB to send patient home, all the way to the other end with the unstable and unflattering "bleeding from both ends" presentation and what we can throw at it (including the kitchen sink) to buy our patients time to definitive management. |
CLINICAL DECISION RULES
35yo male medical student with 2 days of intermittently vomiting bright red blood and non-specific periumbilical pain without a history suggestive of ulcer or varices.
How will you decide on disposition?
Clinical decision rules (or as some countries call it...Clinical Prediction Rules) are tools that quantify individual contributions from history, exam and/or investigations to a likely outcome (in this case death). We use them in clinical practice quite a bit (just look at the number of formulae on mdcalc.com). Some of the more 'mainstream' ones include the PERC criteria, Canadian C-spine rules, ABCD2 score and CHADS-VASC score.
CDRs are often formulated through retrospective analysis of a large pool of data (some might call it educated data dredging) and then prospectively trialled. If the prospective study proves the CDR is worthy, early adopters (and those with superior clinical gestalt - we'll talk about this later) will take it on board (eg...age adjusted d-dimer)(1). However, before CDRs are ready for prime-time the medical population inherently require at least ONE robust validation trial.
"Gestalt"...what's that?
Simon Carley puts it best by calling it "...a sensory interpretation that is greater than the sum of it’s parts". I'd go further to insist that it actually implies a certain expertise in this 'sensory interpretation'. So then what's it got to do with CDRs? A lot. For starters, questions such as "Is PE the number one or equal most likely diagnosis" will vary between an intern and senior specialist. Equally, the most common PEs found in d-dimer negative patients are through gestalt. Indeed, the common theme with all these CDRs (or at least in the discussion part of these articles) is that these scoring systems can be overruled by the clinicians concerns. You can read more about gestalt on the St Emlyn's blog here.
| Rockall (1996) (1) The original, included endoscopy findings (the "Full" Rockall) and later refined to the "Modified" Rockall to maintain purpose in DEM | AIMS65 (2011)(2) An 'easy-to-remember' CDR that has recently been found to be less superior to the GBS (5) |
Published at the turn of this century and maintains its purpose today with multiple powered validation studies (4)(5)
- Used strict conditions to 'rule-out' risk of 30-day mortality
- Phase 1 retrospective, n=61, no adverse effects
- Phase 2 prospective, n = 1748 (22% GBS 0 but 60% not scoped - not lost to follow up), 1 mortality (case review revealed it was not UGIB related)
- Validation studies in 2009 (4) and 2014 (5) continued to show 0% deaths and 0% interventions at 1 month follow up
| Low Risk GBS Criteria (must fulfill ALL) (3)
|
THERAPIES: THE EVIDENCE
- Volume
- Bleeding: physiological & anatomical
- Others: Abx, intervention
| Villanueva (2013)(6)
| Jairath (TRIGGER) (2015)(7)
|
Acid Suppression
Theory
- The UGIT is acidic, blood doesn’t clot in acidic environment (in vivo study suggest ph 6 = 0% clotting, pH 6.57 = 20% clotting)
- Is pH event a good proxy for coagulation?
The Two most referenced papers when it comes to PPI in undifferentiated UGIB:
| Daneshmend (1992)(8)
| Lau (2007)(9)
|
- No change in mortality
- Statistically significant difference in morbidity if given PPI - less scopes, less interventions
| Asian Populations
| The Cochrane review (10) had a look at all the literature taken place in asian populations (of which the Lau (9) study above contributed to mostly) and found:
|
| Non-Asian Populations
| There were 3 notable studies in the Cochrane review (10) that were included in the non-asian subgroup analysis: 1. Daneshmend (8)
2. Hasselgren (11) n = 333
3. Schaffalitzky (12) n = 274
|
What does this all mean about the non-asian population? There might be a higher mortality in non-asian populations (after-all, one standard committee was worried enough to stop two studies)? It's difficult to say - what if the Hasselgren study was allowed to proceed to completion - what the mortality in the last quarter of recruitment even out the statistics and make it non-significant? We just don't know, but will we ever? |
- From the CRASH-2 trial (13) there has been much interest in it's use with every permutation of haemorraghic shock
- A 2014 Cochrane review (14) showed no mortality difference nor any difference in thromboembolic events (n = 1048 over 3 trials)
- No significant difference in thromboembolic events: TXA group (MI+PEx2+CVAx1+DVTx6) vs Control (MIx2+CVAx2+DVTx2)
- HALT-IT is an RCT specificcaly looking at the role of TXA in UGIB, aiming for n=8000 with timeframe of 2017 wrap-up
| The breakdown of thromboembolic events from the review
|
- Permissive hypotension - no literature specific to UGIB
- Restrictive transfusion (ie aim Hb 70)
The following are SPECIFIC for VARICEAL bleeding only
Somatostatin/Octreotide
- Inhibits the release of vasodilator hormones such as glucagon, indirectly causing splanchnic vasoconstriction and decreased portal inflow (decreases portal flow and portal venous pressure). Also inhibits gastric secretion.
- Octreotide is more potent than somatostatin
- Cochrane Review (15) showed no change in mortality but a reduction in 1/2 unit PRBC, though is still found in most protocols
Vasopressin/Terlipressin
- Cochrane Review (16) included 1609 patients in over 20 trials of variable quality
- 6.8% Absolute Reduction (CI 0.49-0.88)
- Vasopressin causes peripheral necrosis, arrythmias and AMIs wheras Terlipressin is a vasopressin analogue with relative specificity for the splanchnic circulation
Other
Antibiotics
- Cirrhotic patients have impaired immune response + GIT bleeding = breach of innate immune system leads to high risk of sepsis in this population
- Cochrane review (17) included 1241 patients in 17 trials of variable quality with no particular consistent antibiotics regime
- ARR 4.7% ie 1 in 22
- Endoscopy
- Surgery
- Interventional Radiology
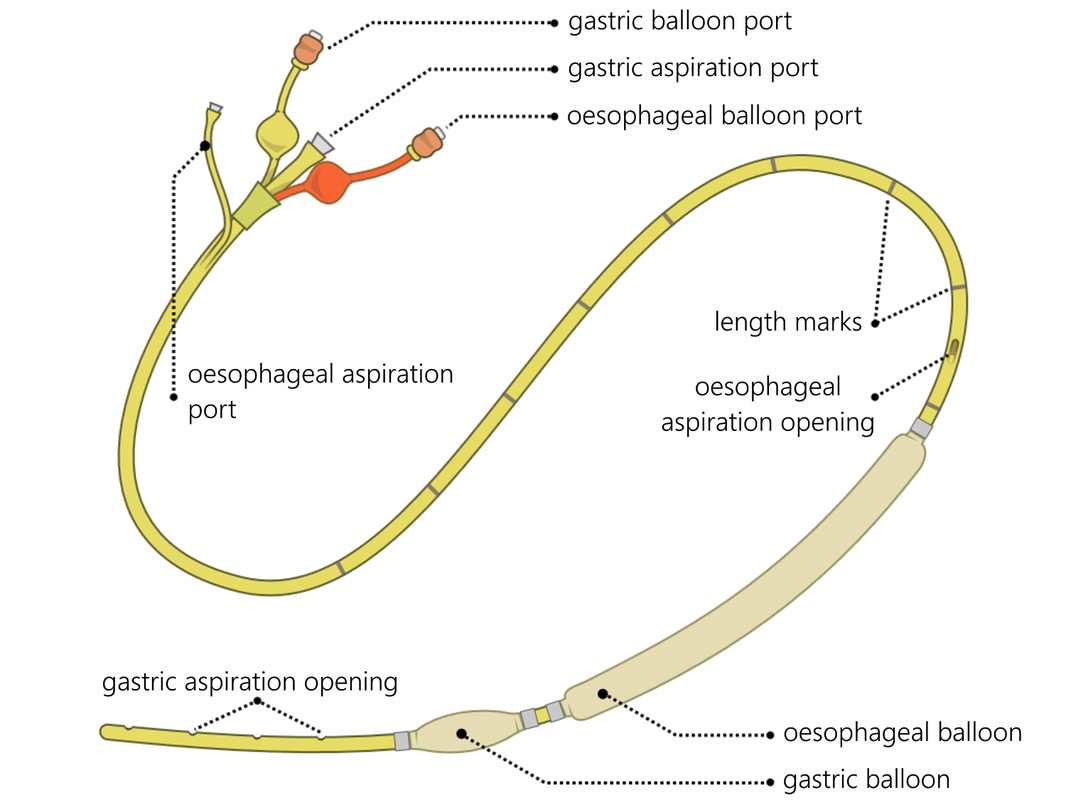
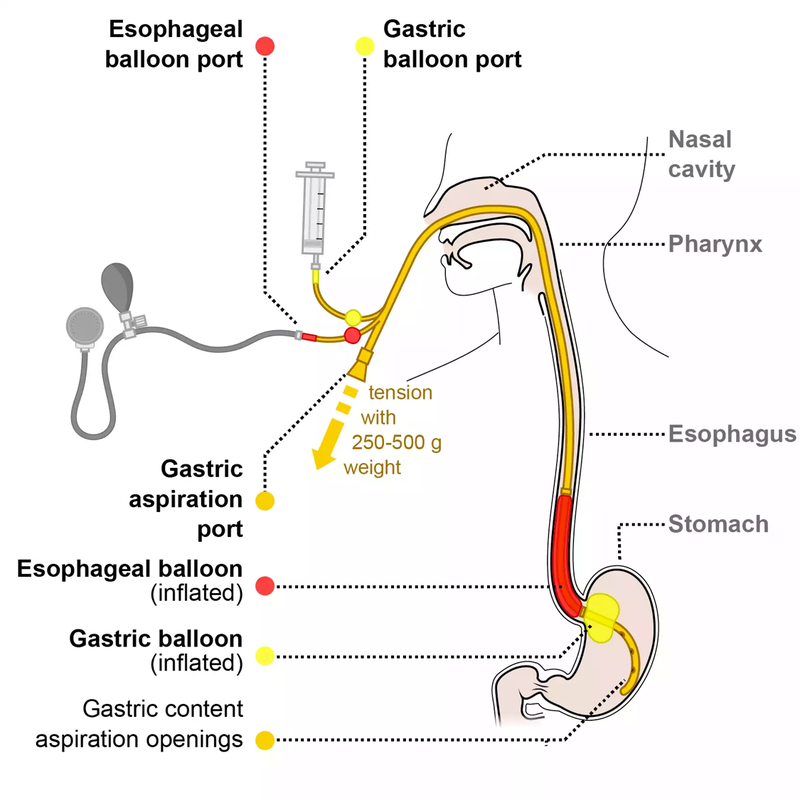
| Despite your best efforts to resuscitate/stabalise a patient, what else can you do to "buy-time" to definitive management? The Senstagen blakemore tube
|
- Rockall TA, Logan RF, Devlin HB, Northfield TC. Risk assessment after acute upper gastrointestinal haemorrhage. Gut. 1996;38(3):316-321.
- Saltzman JR, Tabak YP, Hyett BH, Sun X, Travis AC, Johannes RS. A simple risk score accurately predicts in-hospital mortality, length of stay, and cost in acute upper GI bleeding. YMGE. Elsevier Inc; 2011 Dec 1;74(6):1215–24.
- Blatchford O, Murray WR, Blatchford M. A risk score to predict need for treatment for upper-gastrointestinal haemorrhage. The Lancet. 2000 Oct 14;356(9238):1318–21.
- Stanley AJ, Ashley D, Dalton HR, Mowat C, Gaya DR, Thompson E, et al. Outpatient management of patients with low-risk upper-gastrointestinal haemorrhage: multicentre validation and prospective evaluation. The Lancet. Elsevier Ltd; 2009 Jan 3;373(9657):42–7.
- Yaka E, Yılmaz S, Özgür Doğan N, Pekdemir M. Comparison of the Glasgow-Blatchford and AIMS65 Scoring Systems for Risk Stratification in Upper Gastrointestinal Bleeding in the Emergency Department. Mark Courtney D, editor. Acad Emerg Med. 2014 Dec 31;22(1):22–30.
- Villanueva C, Colomo A, Bosch A, Concepción M, Hernandez-Gea V, Aracil C, et al. Transfusion Strategies for Acute Upper Gastrointestinal Bleeding. N Engl J Med. 2013 Jan 3;368(1):11–21.
- Jairath V, Kahan BC, Gray A, Doré CJ, Mora A, James MW, et al. Restrictive versus liberal blood transfusion for acute upper gastrointestinal bleeding (TRIGGER): a pragmatic, open-label, cluster randomised feasibility trial. Lancet. 2015 Jul 11;386(9989):137–44.
- Daneshmend TK, Hawkey CJ, Langman MJ, Logan RF, Long RG, Walt RP. Omeprazole versus placebo for acute upper gastrointestinal bleeding: randomised double blind controlled trial. BMJ. 1992 Jan 18;304(6820):143–7.
- Lau JY, Leung WK, Wu JCY, Chan FKL, Wong VWS, Chiu PWY, et al. Omeprazole before endoscopy in patients with gastrointestinal bleeding. N Engl J Med. 2007 Apr 19;356(16):1631–40.
- Sreedharan A MJLGDSHCFDMP. Proton pump inhibitor treatment initiated prior to endoscopic diagnosis in upper gastrointestinal bleeding (Review). 2014 Jan 1;:1–73.
- Hasselgren G, Lind T, Lundell L, Aadland E, Efskind P, Falk A, et al. Continuous Intravenous Infusion of Omeprazole in Elderly Patients with Peptic Ulcer Bleeding Results of a Placebo-Controlled Multicenter Study. Scand J Gastroenterol. 1997 Jan;32(4):328–33.
- De Muckadell OBS, Havelund T, Harling H, Boesby S, Snel P, Vreeburg EM, et al. Effect of Omeprazole on the Outcome of Endoscopically Treated Bleeding Peptic Ulcers Randomized Double-Blind Placebo-Controlled Multicentre Study. Scand J Gastroenterol. 1997 Jan;32(4):320–7.
- Collaborators TC-2. The importance of early treatment with tranexamic acid in bleeding trauma patients: an exploratory analysis of the CRASH-2 randomised controlled trial. The Lancet. Elsevier Ltd; 2011 Mar 26;377(9771):1096–1101.e2.
- Bennett C KSLEGL. Tranexamic acid for upper gastrointestinal bleeding (Review). 2014 Jan 1;:1–64.
- Alhazzani W WLHCLG. Somatostatin or somatostatin analogues for acute non- variceal upper gastrointestinal bleeding (Protocol). 2013 Jan 1;:1–12.
- Gotzsche PC HA. Somatostatin analogues for acute bleeding oesophageal varices (Review). 2014 Jan 1;:1–35.
- Chavez-Tapia NC B-GTT-AFS-WKUM. Antibiotic prophylaxis for cirrhotic patients with upper gastrointestinal bleeding (Review). 2014 Jan 1;:1–44.
- Clinical Decision Rules as a 'ball park' to refine "gestalt" - GBS rules in UGIB
- Mortality Benefit: Transfusing < 70Hb, Antibiotics (variceal), Terlipressin (variceal)
- Morbidity Benefit: PPIs, Octreotide (variceal)
- The Horizon: TXA (HALT-IT trial)
- All roads lead to definitive management (not the Senstagen Blakemore Tube!)


 RSS Feed
RSS Feed
