Otherwise well recently, no sick contacts, no exotic travel history.
Associated symptoms; no chest pain, syncope or palpitations, maybe some left thigh pain but only on prompting
A distant history of what sounds like an unprovoked DVT with unclear follow up but hasn't been on "the rat poison" for years.
| Looks dreadful! Cyanotic but talking in short phrases RR 70 Sats 84% RA (89-91% 15L NRBM) BP 96/48 HR 120 Afebrile | Good AE (when she can) HSD NM JVP approx 6cm Calves SNT without pedal oedema |
Such sudden drastic deterioration is likely due to a heart (AMI), lung (PXT) or vascular problem (PE, Dissection in coronaries).
And sepsis...sepsis is always on the radar
Bedside
ECG - Sinus Tachy, maybe some R heart strain but definitly nothing to catheterise at this stage
VBG - machine broken, being sent to the lab
BSL - 9
Cxr - radiographer on the way
The patients sick and the decision is made for CT to rule out the immediate life threats in the not-so-good looking patient.
CT
So what are we going to order? Non-Con vs CTPA vs Aortagram vs CTCA? The hooves sound like horses so lets go with the CTPA...
Occlusive thrombus in R main pulmonary artery (shown image 1)
Thrombi in L lobar pulmonary arterial branches
Evidence of R heart strain
Flattening of the interventricular septum
Reflux of contrast into the hepatic arteries and IVC (shown image 2)
American Heart Association Grading
| MASSIVE SBP< 90mmHg (15mins or ionotropes) OR Profound bradycardia with signs of shock OR Pulselessness (this is bad) | SUBMASSIVE SBP>90mmHg with evidence of RV dysfunction (on CTPA, Echo or "Biomarkers") | NON-MASSIVE Everything else! |
SBP > 100mmHg + CTPA shows RV dysfunction + Oh, and the bloods are back...hsTn 119 = SUBMASSIVE
Nothing or Anticoagulant or Lyse (systemic or interventional radiology) or Embolectomy or Nothing
| Some Evidence Around Lysis... | (click on pictures for articles where available) |
| Fibrinolysis for Patients with Intermediate-Risk Pulmonary Embolism (PEITHO Trial) 2014
NNT 33 vs NNH 13.7 Trend toward decreased mortality (non-sig) but increased bleeding (non-sig). Does not support thrombolysis in submassive PE | Moderate Pulmonary Embolism Treated With Thrombolysis (from the “MOPETT” Trial) 2013
ARR 41%, NNT 2.4 Difficult to interpret study as measured echocardiographic outcomes | Systematic review and meta-analysis for thrombolysis treatment in patients with acute submassive pulmonary embolism. 2014
|
- There is a role for thrombolysis in submassive PE.
- The ‘Submassive’ group is too disparate to find an effect based on current definitions.
Named after the practitioner who provided most of the above information, it is a stream of consciousness that consolidates the evidence and the stuff between the lines
- Some "submassives" are on the way to being massive
- Thrombolysis zeal post N=1 has deflated
- Still a little confused but less than before
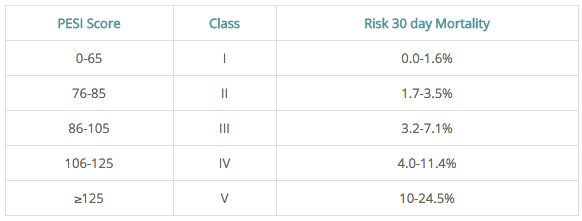
PESI (Pulmonary Embolism Severity Index) scores 30 day mortality (does not include all the following)
| Suggested Interpretation of Score Very Low (≤ 65) or Low Risk (66-85) by the PESI score.
|

 RSS Feed
RSS Feed
