- The 3 most important factors in DCI are the 3 "D's": Depth, Duration & Decompression
- The earlier the onset, the more severe (and neurological) it is likely to be
- The majority of DCI occurs within table limits and is due to individual susceptibility (and remember, DCIEM tables are deterministic not probabilistic, therefore risk of DCI higher as you go down and to the right of the table - starts at around 2-3%)
- Depth: depth correlates to pressure, with more pressure causing more dissolved gas and without appropriate deco - more bubbles on ascent
- Duration: with more time under pressure comes more dissolved bubbles...
- Decompression: Remembering that deco-tables are modelled within a 2-3% risk, the closer you are to deco-limits (the right of the table), and the lower down you go (depth), increases your risk - a risk that individual-to-individual is in itself variable. Also, uncontrolled ascent must be assumed if anything has happened in the water eg "i lost my dive buddy so i surfaced in a controlled manner"
Other factors that may should ring alarm bells for anyone suspicious of DCI (in addition to the 3 D's) include:
- Multiple dives
- Ascent to altitude post dive
- Exercise during or after dive
- Gas mixtures
- Heat
- Depth, duration, decompression
- What was the onset? acute and profound suggests CAGE, all else suggests DCS
- What were the symptoms? Was it a discrete, combined or fulminant DCS picture - this helps to determine management later on
- How did the symptoms progress? A sudden onset-sudden offset pattern suggests CAGE (where bubble are no longer impeding discrete flow), all else suggests DCS (where bubbles cause endothelial narrowing through inflammation, something not readily reversible)
- Was anyone else sick? Might suggest 'dirty gas'
- Were symptoms precipitated with straining? This may suggest embolisation from barotrauma or a PFO
- Position: supine (previously advocated to be 30 deg head down to stop bubbles going to the head, but simplified to supine position now. Head down can also exacerbate right heart pressure and cause more bubbles going through a PFO if that's the cause of the bubble disease)
- Oxygen: aim for an FiO2 of 100% (note that a NRB gets about 80%, BVM @ 15L/min is your best, non-hacked bet)
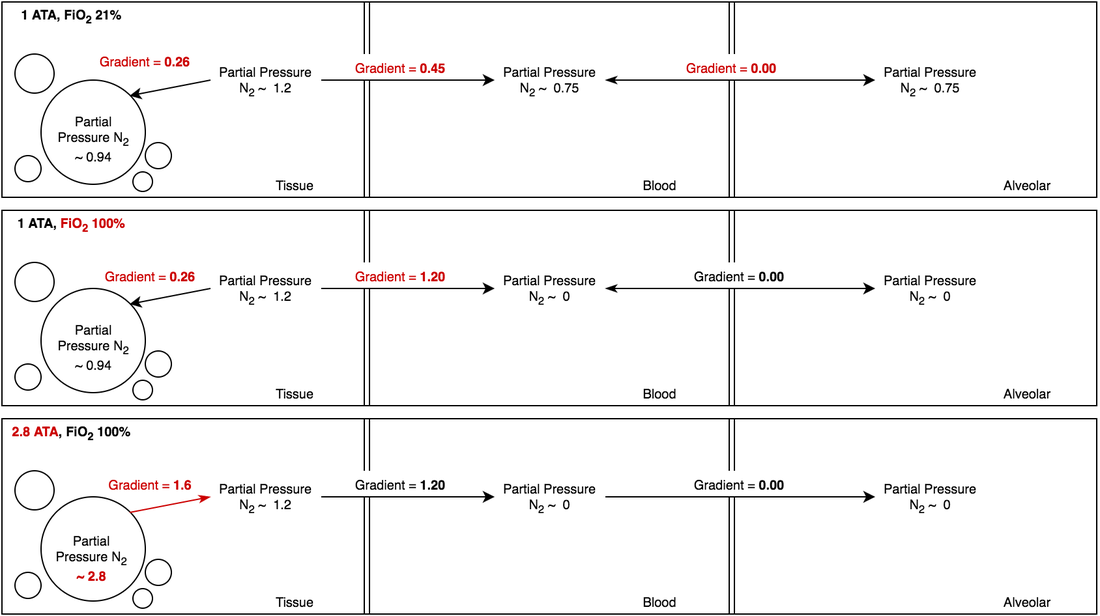
- Why it works - provides a bigger tissue-blood gradient and blood-alveolar gradient for gas to diffuse out of (see fig below)
- Note that there is still a gradient INTO bubbles (which we will soon see, is reversed with hyperbaric therapy)
- Fluids: maintain adequate circulating volume (remember that pressure & cold temp causes centralisation of blood leading to bigger preload, which releases ANP causing a diuresis)
- Anti-inflammatory: more relevant for the DCS with the bubble mediate endothelial injury
- Environment: keeping the diver warm will increase circulating blood to areas that need to off-gas as well as hasten it
- Exercise: minimise exertion to prevent more bubbles from both dissolved state going through a PFO & barotrauma
- Urgency depends on where on the spectrum of DCI that the patient lies (and access to a hyperbaric chamber)
- Limit altitude to 150m (300m max) - since altitude decreases pressure, this increases bubble formation, therefore it would be wise to restrict
- Most planes will be able to pressurise to 1 ATA
Delay to Treatment & Outcomes for Spinal DCS
- < 3 hrs: 76% full recovery, 24% sequelae
- 3-6 hrs: 82% full recovery, 18% sequelae
- > 6 hrs: 63% recovery, 37% sequelae
- Ideally in a facility with intensive care hyperbaric facilities
- ABC's & H (for hyperbaric oxygen therapy - HBOT)
- Regardless of depth profile, all comers are re-compressed using the "RN62" table (see later for a mostly academic discussion of alternative tables that can be used)
- Delays to treatment < 6 hrs all have similar efficacy for recovery, 12-48 hrs less so and beyond 48hrs unlikely any
Complications of HBOT
- Barotrauma (inner/middle/outer ears, sinuses, pulmonary, gastric)
- Toxicity: O2, N2, CO2, He
- Exacerbation of conditions eg PTX
- Claustrophobia
- Disease progression
- Retinopathy & lens changes with chronic application
- Limited intervention restricted by chamber movements
Adjuncts to Hyperbaric Oxygen Therapy
- Fluids
- NSAIDs
- Maybe benefit: lignocaine infusion for CAGE
- Unlikely benefit: steroids, aspirin, heparin
Between HBOT Sessions
- No O2 - unless clinically indicated otherwise may precipitate O2 toxicity
- Unless dire, can usually be done as an 'outpatient'
- The usual flying/diving restrictions whilst not in the chamber
- Minimal exercise to prevent more bubbles going to the wrong places
- Gradually return to normal activity
- Report any relapses
- Avoid altitude > 300m and flying for at least 1 week (although 1 month is preferred - especially if more severe form of DCI)
- Follow up in 1 month for a diving medical
- Suspected pulmonary barotrauma (PB) is an absolute contraindication - remember that not even a high res CT can find changes that predispose to PB: fool me once, shame on you; fool me twice, shame on...
- Workup for a PFO if indicated (DCS either spinal, cutaneous, cerebral or inner ear)
- Generally ok to return to water after 1 month if symptom free and passes usual dive medical requirements


 RSS Feed
RSS Feed
