| Viet Tran It's 7:15AM and you've got the department in ship shape to handover...for once. "Cat 2 Resus 2" - great, its another chest pain...the night brain urges your type 1 thinking into gear (dont even talk about type 2 after the night you had)...history, examination, ecg, serial Tn...the day team can sort the rest out... |
You stroll into Resus 2 and are greeted by the ambulance officer off loading a 72yo female short of breathe looking uncomfortable in the chest.
"This is Gladys, she woke up an hour ago with chest pain, tried to eat some toast thinking it was her indigestion but fell to the floor after feeling faint. She was too weak to get up so she pressed her personal alarm. We turned up, gave her some aspirin, 2 sprays of GTN and 5mg of morphine which eased the pain, but it seems to have come back transferring her over to the bed. The ECG looks funny...not sure if its old, Gladys says this has happened before and she had a pacemaker inserted. She's remained stable en route".
There's not much more history that Gladys can offer nor collateral.
She looks appropriate for her age, talking in short sentences and uncomfortable in the chest without looking dreadful.
HR 63 regular / Sats 99% RA / RR23 / T36.7 / GCS 15
HS dual and unsure if anything added because your nurses are trying to get that ecg you asked for.
She has no evidence of cardiac surgery but you can palpate an internal cardiac device over her left superior chest.
Lungs generally clear also.
Gladys has bilateral pedal oedema up to her thighs which she says has been there for the last few months
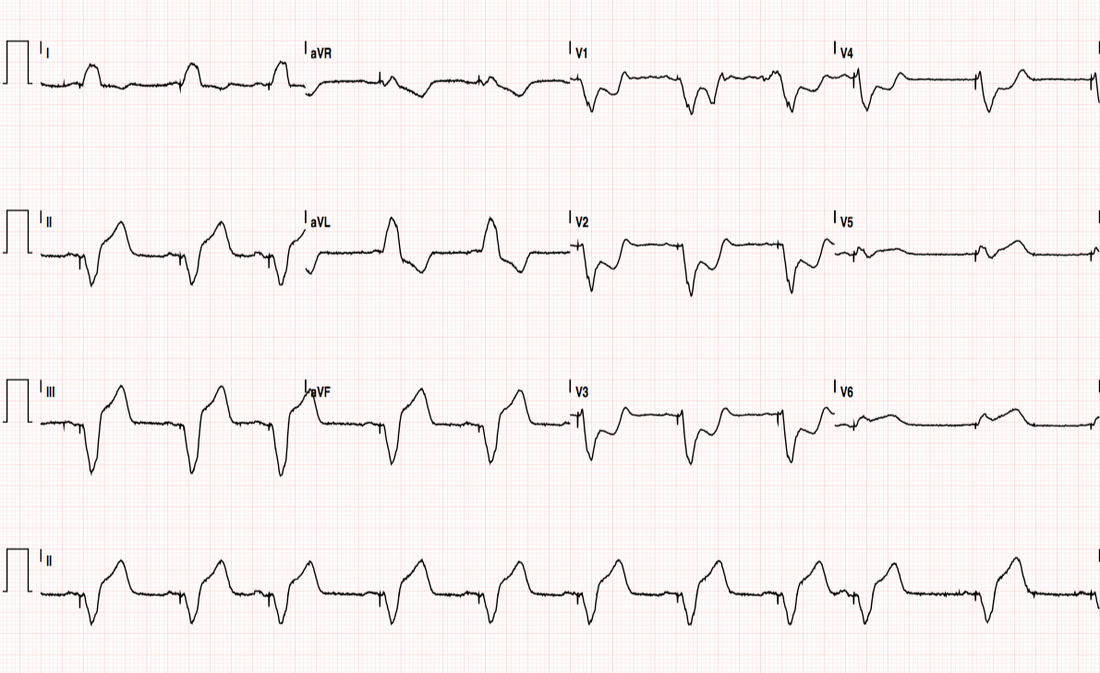
The nurse hands you the ECG as you request more GTN and Fentynl...
1. Ventricular Paced Rhythm (pacing spikes visible) at 63BPM
2. Cant interpret because its a paced rhythm...hope someone from the day team turns up early...might look at the patient to see how she's going...
Looks unchanged, but not great looking
Better take another look at that ECG...
Didn't the senior reg say something about "interpreting the uninterpretable" at teaching the other month? Sarcophagus? Smoboso? Barossa? Garboso? Sgarbossa!
What is it again?
- Used to interpret STEMI-equivalents in LBBB or ventricular paced rhythms...perfect!
- The original Sgarbossa Criteria is 98% specific for a STEMI equivalent if ≥3 points (but 52% sensitive - as low as 20% in some studies (3, 4))
- The modified Criteria improves on the sensitivity (91%) but is less specific (90%) (2)
| Original Sgarbossa Criteria (1)
| Modified (Smith) Sgarbossa Criteria (2)
|
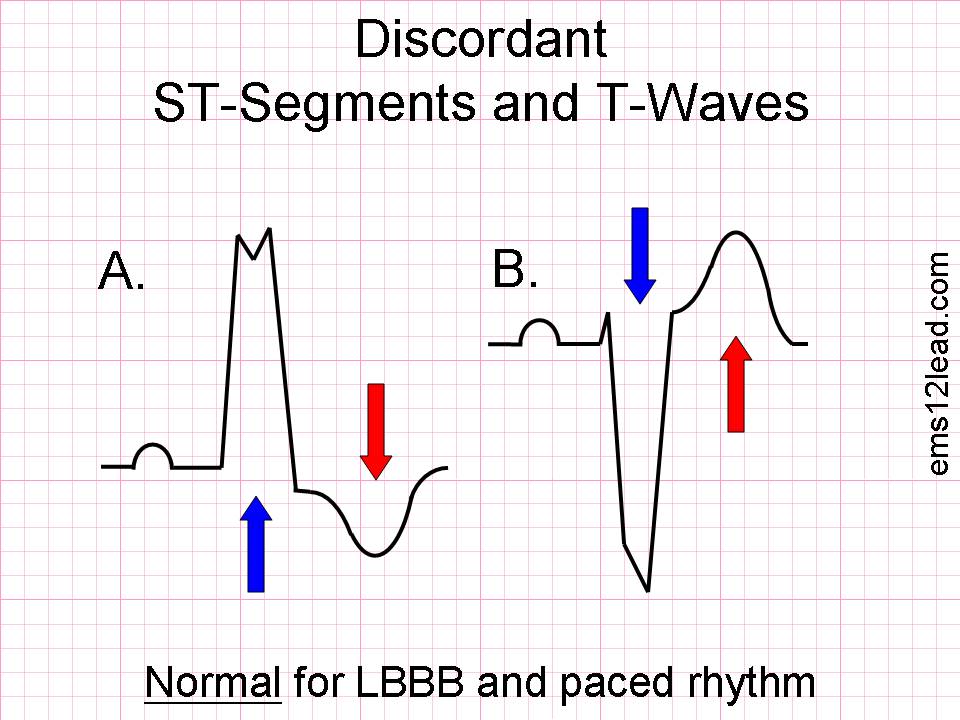
In this case concordance and discordance describe the relationship of the QRS to the ST segment
| With a normal ECG we expect the ST segment to be isoelectric. With LBBB or Ventricular paced rhythms, the ST segment is not isoelectric, instead, it is expected to be either elevated or depressed in the opposite direction to the QRS complex. Thus the QRS/ST relationship is discordant. A. Shows that the QRS is a POSITIVE deflection and therefore the ST segment should be a NEGATIVE deflection B. Shows that the QRS is a NEGATIVE deflection and therefore the ST segment should be a POSITIVE deflection |
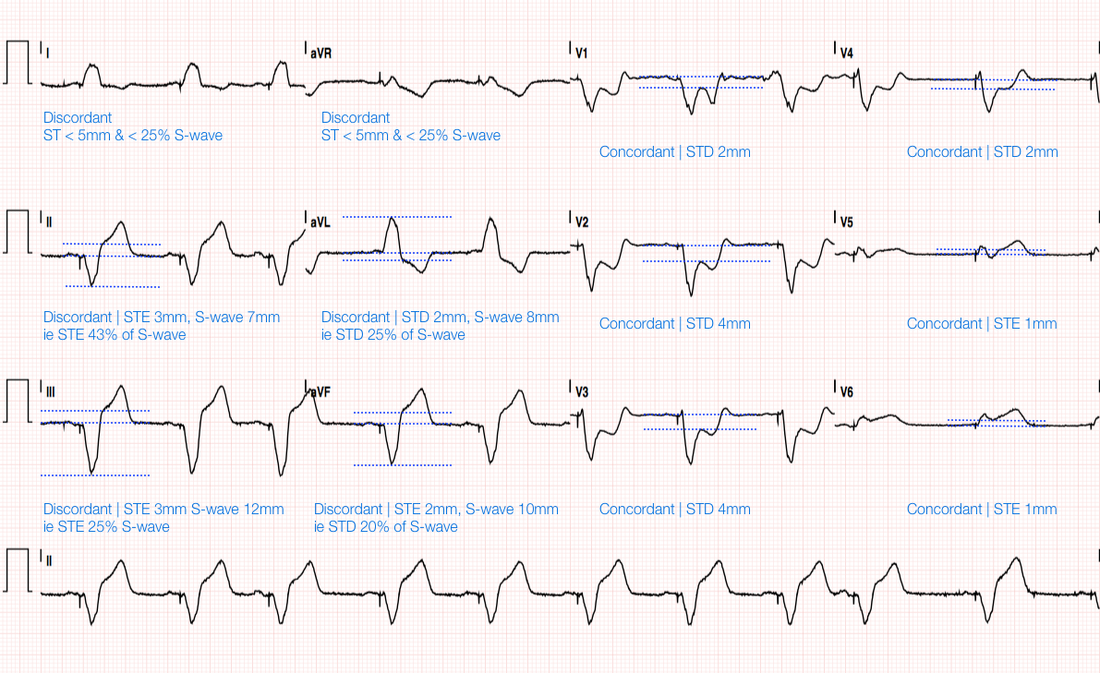
Rather than go through the Sgarbossa Criteria lets work out if each lead is discordant or concordant. If they are Concordant than we can check if they are elevated or depressed, If they are discordant than we can check if it is > 5mm (original) or > 25% of the S-wave
So let go through the leads:
- Concordant ST elevation > 1mm in any lead (5 pts) = V 5-6
- Concordant ST depression > 1 mm in V1-V3 (3 pts) = V 1-4
- Discordant ST elevation > 5 mm in any lead (2 pts) = Lead II, III dont quite meet criteria
With the modified criteria it's even more convincing that Gladys has had a STEMI
- Concordant ST elevation ≥1 mm any lead = V 5-6
- Concordant ST depression ≥ 1 mm in lead V1-V3 = V1-4
- Discordant ST/S Ratio > 0.25 of S-wave = Lead II & III
Get Gladys to the cath lab...CODE STEMI!
Heres a list of STEMI equivalents not to miss
- Wellen's Syndrome
- Sgarbossa Criteria
- DeWinter's T-waves
- Posterior MI
- LMCA Occlusion
NB NEW LBBB is no longer considered a STEMI equivalent
- Sgarbossa E, et al.. "Electrocardiographic diagnosis of evolving acute myocardial infarction in the presence of left bundle-branch block. GUSTO-1 (Global Utilization of Streptokinase and Tissue Plasminogen Activator for Occluded Coronary Arteries) Investigators". NEJM. 1996; 334(8):481-7
- Smith, S, et al. Diagnosis of ST-Elevation Myocardial Infarction in the Presence of Left Bundle Branch Block With the ST-Elevation to S-Wave Ratio in a Modified Sgarbossa Rule. 60(6):766-776.
- Chang AM, Shofer FS, Tabas JA, Magid DJ, McCusker CM, Hollander JE. Lack of association between left bundle-branch block and acute myocardial infarction in symptomatic ED patients. Am J Emerg Med. 2009; 27(8): 916-21.
- Jain S, Ting HT, Bell M, et al. Utility of left bundle branch block as a diagnostic criterion for acute myocardial infarction. Am J Cardiol. 2011; 107(8): 1111-6.


 RSS Feed
RSS Feed
