A 59yo female, out of hospital cardiac arrest arrives with ROSC.
Your primary survey includes:
C. No catastrophic bleeding
A. Supraglottic airway (in this case, an iGel)
B. Sat 92% on FiO2 100% via a BVM connected to the iGel
C. HR 120, NIBP 170/110 unsupported pharmacologically
D. GCS 3, no evidence of trauma, pupils 3 sluggish bilateral
The team leader is organising resuscitation, diagnosis & disposition in parallel. You were pre-allocated the role of airway doctor & prepare for intubation. Once the team is ready you do a slick first pass intubation with a grade 1 view & without any haemodynamic or oxygenation hiccups.
Tube placement is confirmed by ETCO2, fogging of the tube & bilateral lung auscultation. X-ray are on their way. You connect the patient to the ventilator to free yourself a little.
11 minutes pass & the disposition is cath lab, with the team now setting up for transfer. As you look up you noticed that the Sats have fallen from 92% post intubation to 86% - and you have yet to dial down your FiO2 from 100%...
How do you approach this issue?
At any stage has the tube been dislodged? Check your surrogates for correct position - Is there still fogging of the tube? Has the ETCO2 changed? Can you still hear breath sounds bilaterally? If need be, re-paralyse the patient & use your laryngoscope to have a direct view. Oh, and where's that x-ray?
Is the patient hard to bag? Can you put a suction catheter down - any muck coming up? Perhaps they aspirated prior to intubation (even pre-hospital). A change from negative pressure ventilation to operator controlled positive pressure ventilation (PPV) can sometimes upset a fine balance of auto regulation, once taken away with muscle relaxants & sedative.
Have you blown a lung or made a small pneumothorax bigger with your PPV? Ausculate, USS, X-ray & stick a needle (or tube) in it if you find it.
Is it the ventilator? Disconnect & hand bag - get a feel for the compliance & remove the ventilator variable out of the equation. Is the pulse ox correct or are those sats for the bed sheets? A blood gas can help confirm the desaturation if you have the time & still haven't worked it out.
Is this patient at risk of breath stacking (asthma, COPD, ventilator settings) - do they need a period of no PPV? Was the desaturation preceded by ignored high pressure alarms on the ventilator?
O - no issues with air in/out, suction clear
P - breathe sounds both sides, rattly left lower zone, USS/X-ray pending
E - Disconnected from ventilator, hand bag with PEEP valve, a little firm...
S - Not suspicious for stacking, no hx of asthma/copd, vent settings were liberal
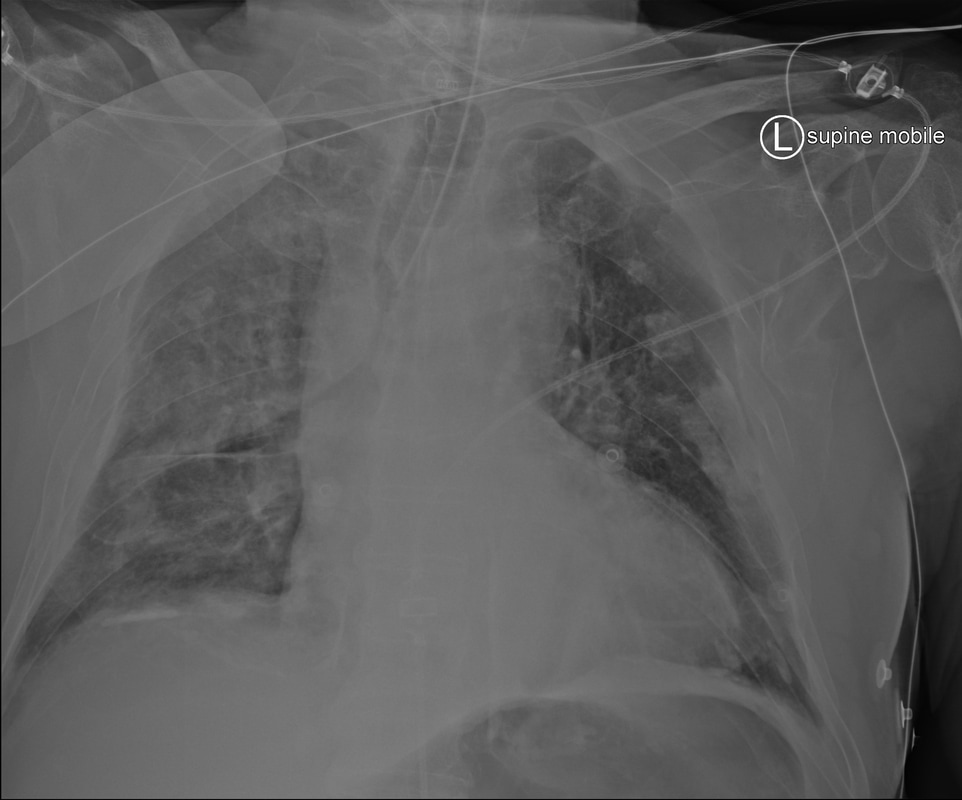
X-ray rolled up & showed:
After a bit of hand bagging with a cranked up PEEP valve & in the context of the above x-ray, the sats come back up. Looks like she had a profound VQ mismatch & with the change in dynamics of lung ventilation her artificial compensatory mechanisms (i.e. us adjusting things like minute ventilation, volume, PEEP...) was no match for her auto-regulation. Once found, then fixed. DOPES.


 RSS Feed
RSS Feed
