- Majority of renal stones will spontaneously pass
- NSAIDs first line for analgesia
- Use IV fluids for dehydration, not expulsion
- Supportive expectant care is mainstay
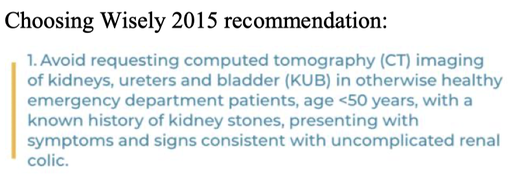
- CT KUB seems to be our go-to imaging – could be starting with US in selected lower risk patients to minimise harms, however in our group discussion we noted many barriers to this
- Evidence on tamsulosin is mixed
- Common condition: lifetime risk estimates ~12% males & 6% females
- 75-90% of stones will pass spontaneously
Review of evidence & guidelines
Analgesia
Three large systematic reviews & meta-analyses about drug class:
1. 2004 Cochrane: NSAIDs vs. opioids (20 RCTs, n = 1613)
- Both significantly reduce pain, in some studies lower pain scores w NSAIDs
- More adverse effects (e.g. vomiting) with opioids
2. 2015 Cochrane: NSAIDs & non-opioids (50 RCTs, n= 5734 participants)
- Combination of NSAIDs + antispasmodics was not superior to NSAIDs only
- Data on other non-opioid, non-NSAID medication scarce
3. 2018 European Urology: NSAIDs, opioids & paracetamol (36 RCTs, n = 4887)
- Pain reduction at 30 mins w NSAIDs equivalent to opioids or paracetamol
- “Despite observed heterogeneity among the included studies and the overall quality of evidence, the findings of a lower need for rescue analgesia and fewer adverse events, in conjunction with the practical advantages of ease of delivery, suggest that NSAIDs should be the preferred analgesic option for patients presenting to the emergency department with renal colic.”
Choice of NSAID
- A few small RCTs comparing NSAIDs for renal colic (IM ketorolac vs. diclofenac; IV ketorolac vs ibuprofen): similar reduction in pain scores, low rates of adverse outcomes, less GI side effects with ketorolac
- No strong evidence ketorolac is better than other NSAIDs, but benefits include IM route in vomiting and no suggestion it is less efficacious or less safe. Many guidelines recommend PR indomethacin rather than IM ketorolac.
IV Fluids
2012 Cochrane review: only 2 RCTs, no reliable evidence to support “forced fluid” strategy.
“Significantly dehydrated patients with vomiting may require replacement +/- maintenance IV fluids, but fluid administration is not routine therapy for renal colic as it does not facilitate stone passage and may worsen pain secondary to renal capsular distension.”
- Emergency Care Institute, NSW
Investigations: UA
Sensitivity of haematuria on microscopic urinalysis for renal colic using CT as reference standard 84% (Luchs 2002); more recent studies incidentally found up to a third had no haematuria on UA.
Investigations: Imaging
Smith-Bindman et al. 2014 – important study on initial ED imaging modality
- Multi-centre, pragmatic, comparative effectiveness trial, n = 2759
- Randomised to POCUS/ formal US/ CT KUB as initial imaging method
- Found return ED visits, hospitalisations & diagnostic accuracy did not differ significantly between groups, with low incidence of high-risk diagnoses with complications within 30 days (0.4%) across all modalities
- 6-month cumulative radiation exposure significantly lower in US groups (however 41% still got a CT KUB later on)
Wong et al. 2019 meta-analysis of accuracy and prognostic value of POCUS:
- 5 studies,n=1,773
- Sensitivity & specificity for detecting stone were 70.2% (95% CI 67.1%–73.2%) & 75.4% (95% CI 72.5%–78.2%)
- Finding of moderate or severe hydronephrosis highly specific (94.4%) for the presence of any stone, and the presence of any hydronephrosis is suggestive of a larger (>5 mm) stone
Moore et al. 2019 – consensus from US Colleges for Emergency, Radiology & Urology:
- “Evidence and multispecialty consensus support ultrasound or no further imaging in specific clinical scenarios, with reduced-radiation dose CT to be employed when CT is needed in patients with suspected renal colic.”
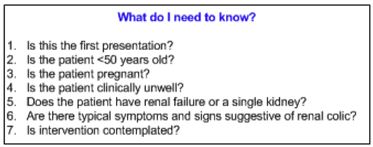
Several Australian guidelines; WA Diagnostic Imaging Pathways (2015) is a flow chart based off seven questions:
- Includes alpha-1 blockers eg tamulosin, calcian channel blockers eg nifedipine
- Rationale: relax ureteral smooth muscle facilitates stone passage decreased pain and decreased need for surgical intervention
- Mixed evidence
- 2008 Seitz et al. meta-analysis of alpha blockers + calcium channel stabilisers found MET increased likelihood of spontaneous stone passage (RR 1.45)
- 2012 Cochrane review: alpha blockers increased likelihood of stone passage compared with control (RR 1.48), most evidence for tamsulosin
- Pickard et al. 2015 multi-centre RCT tamsulosin vs. nifedipine vs. placebo (n= 1136): neither drug decreased % patients needing further intervention to clear stone ≤4 weeks; no evidence of reduced pain or faster stone passage
- Emergency Care Institute (NSW): https://aci.health.nsw.gov.au/networks/eci/clinical/clinicaltools/renal/renal-colic
- Emergency Medicine Cases podcast 2015, Ultrasound vs CT for Renal Colic (on SmithBindman et al. 2014): https://emergencymedicinecases.com/ultrasound-vs-ct-for-renal-colic/
- WA Imaging Pathway: http://www.imagingpathways.health.wa.gov.au/index.php/imagingpathways/gastrointestinal/acute-abdomen/acute-flank-loin-pain-renal-colic#pathway
- Choosing Wisely: https://www.choosingwisely.org.au/recommendations/acem
- SGEM podcast 2019, renal colic imaging (on Moore et al. 2019) https://www.thesgem.com/2019/12/sgem-xtra-come-together-right-now-over-renal-colic/

 RSS Feed
RSS Feed
