| Brain Food is a project to drip feed clinical knowledge (in the form of mock SAQs) to satisfy those hungry neurons. Sources are SA/NT Trial Exam 2021.2 and Monash 2022.1. Answers are prone to ageing. Leave a comment if you don't understand or something doesn't seem right... PS we don't use the mock questions uploaded to ACEMs official mocks |
A 53-year-old man is transferred from a rural hospital to your tertiary hospital for worsening respiratory distress.
He was treated for a chest infection for the last 24 hours but developed worsening respiratory symptoms and hypoxaemia.
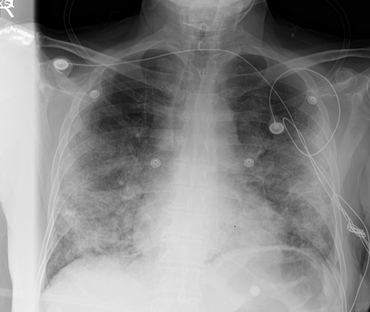
A chest XR is taken shortly after arrival and shown below.
The patient informs you that he is an interstate truck driver and has just returned from the neighbouring COVID-ravaged state 3 days ago. He developed a cough and sore throat the day after he returned but thought it was just a cold and did not seek medical attention.
He was previously well with no significant medical or surgical conditions.
His observations are:
HR 122 bpm
BP 102/64 mmHg
RR 30 bpm
SaO2 81% NRB 15L/min
Temp 39.3C degrees
His ABG shows the following:
pH 7.31
PCO2 52
PO2 81
HCO3 18
2. APO
3. Bilateral Pneumonia
4. Diffuse pulmonary haemorrhage
5. Disseminated malignancy
6. Inflammatory or autoimmune conditions ( acute eosinophilic pneumonia, pulm vasculitis, cryptogenic organising pneumonia, pulmonary fibrosis)
7. Embolic syndromes (fat or amniotic fluid embolism)
2. Full PPE including N95 mask
3. Use the most experienced intubator
4. Video laryngoscopy
5. Avoid ventilation using an open circuit
6. Preoxygenate with BVM with viral filter and two hands vice grip on mask for tight seal.
7. Clamping of the ETT whenever disconnected
8. Use of inline suction device
9. Adequate sedation and paralysis to minimise coughing
2. Avoid high plateau pressure (<30mmHg)
3. Titrate PEEP according to ARDSnet PEEP table or best compliance strategy
4. Permissive hypercapnia (as long as arterial pH >7.2)
5. Avoid hyperoxia (titrate FiO2 to achieve SaO2 92‐96%)
BNP: APO
D-dimer: marked elevation suggests COVID
ECG: may show features of ischaemia/myocarditis or cardiomyopathy
CT chest: typical patterns may differentiate COVID from fibrosis, from other types of infection and from cardiogenic oedema.
Urine: urinary legionella and streptococcal antigens
TTE: may show reduced EF and other features of ischaemia/myocarditis

 RSS Feed
RSS Feed
