| Brian Doyle Our local Guru of EBM, Brian Doyle, hosts a monthly Journal Club for the locals. In the spirit of consolidating knowledge and sharing this with the world, with permission, here is a re-post of one of the articles discussed. For more juicy journals served on a platter, head over to Brian's JC blog: EmergencyMedJc |
Wang, HE, Schmicker RH, Daya MR, et al. Effect of a Strategy of Initial Laryngeal Tube Insertion vs. Endotracheal Intubation on 72-Hour Survival in Adults with Out-of-Hospital Cardiac Arrest. JAMA 2018;320(8):769-778.
This study was a large cluster-crossover clinical trial in the USA attempting to answer this research question. 27 EMS agencies were randomized in clusters to either a laryngeal tube or endotracheal tube with crossover to the alternate strategy at 3 to 5 month intervals.
Why randomize EMS agencies? Wouldn’t it be better to randomise individual patients?
Think feasibility.
Research in cardiac arrest is challenging. The last thing paramedics want to do during a code is open a study envelope. They’ve got other things on their minds. Hence randomise EMS agencies. Of course this can introduce bias and statistical inefficiency. But such is compromise in research.
The primary outcome was 72-hour survival. They did report the much more important outcome of favourable neurologic status (mRS<3) at discharge from hospital.
Results?
3000 patients were enrolled. About half were unwitnessed and/or had no bystander CPR. 80% had non-shockable rhythms. It’s no surprise overall outcomes were terrible. It is also challenging to demonstrate a difference in treatment strategies when the vast majority were going to die regardless of intervention. But such is life… and death.
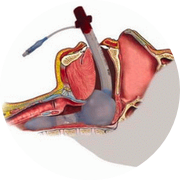
Rates of initial airway success were 90% with the laryngeal tube but a pretty dismal 50% with the endotracheal tube. Yikes!
72-hour survival was 18% with the laryngeal tube and 15% with the endotracheal tube. Rates of favourable neurologic outcome was 7% vs. 5% favouring the laryngeal tube.
What are we to think?
Unfortunately, this study did have some problems. It had poor rates of first pass success with intubation. The pragmatic study design and cluster randomisation introduced noise. They only studied one type of supraglottic airway… i.e. not the LMA.
But in the end, there probably is no compelling reason to push for endotracheal intubationin the field. This may distract from other meaningful interventions such as good quality CPR and rapid defibrillation.
It’s unclear how much of this is externally valid to a well-resourced Emergency Department. A dedicated airway doctor and lots of hands might change our outlook. Nevertheless, this study does push our focus away from the endotracheal tube in cardiac arrest.
About The Author
| Dr Brian Doyle is an emergency physician originally from the United States but now very much calls Tasmania his home. Unfortunately, it will now be a bit more difficult to deport him from the country as he passed his Australian citizenship test a few years ago. (He was able to answer that Phar Lap won the Melbourne rather than the Davis Cup). His main interests are mostly the clinical aspects of emergency medicine but also in education, ultrasound and critical appraisal of the literature. He spends much of his time annoying people to help out with conferences. |


 RSS Feed
RSS Feed
