He was well yesterday with some 'sore muscles' that evolved into feeling 'generally unwell' overnight, not able to sleep with nausea, some vomiting and nondescript abdominal pain.
After not being able to keep anything down today, and being too weak to mobilise on his own to the bathroom, his partner called an ambulance.
His past history includes morbid obesity and type 2 diabetes mellitus.
He's on ozempic and dapagliflozin.
He's seen by triage and assigned a CAT 2 and moved to resus. He looks dreadful.
Heart Rate 120, Blood Pressure 110/70, T37.2, Sat 97%RA, RR42
Appears very dry, with a soft but generally tender abdomen and no other significant findings
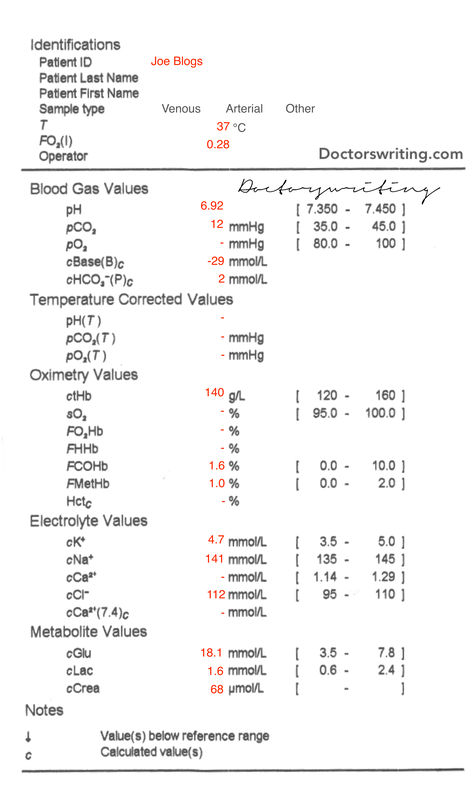
A blood gas is done (below) and ketones were 8.0 mmol/L
Cause of acidosis?
- CO2 = 12 ∴ primary metabolic acidosis
- HCO3 = 2 (critical) also supports primary metabolic acidosis
Is there appropriate respiratory compensation or a concomitant process?
- Expected CO2 = 1.5 x HCO3 + 8 = 11
- Actual CO2 = 12 ∴ appropriate compensation (but also means very tachypneic!)
NB Tachypnoea in the context of a sick looking patient can often reflect mod-severe acidaemia - try and guess the pH of someone you see with tachypnoea and appears unwell next time!
What is the cause of the metabolic acidosis?
- Anion Gap = 141 - 2 - 112 = 27 = HAGMA (normal is 12 +/- 4)
It's a HAGMA, so we should check if there is another concomitant metabolic process:
- Delta Ratio = (27 - 12) / (24 - 2) = 0.68
- DR 0.4-0.8 so this is a NAGMA in addition to the HAGMA
- Actual Na = mNa + (Glc - 5)/3 = 141 + (18.1 - 5)/3 = 145
- ∴ Normonatraemic
K (for pH)
- Expected K = 5(7.4 - pH) +5 = 5(7.4 - 6.92) + 5 = 7.4
- Measured K = 4.7 ∴ relative hypOkalaemia
Ca (for alb)
- Ca not measured, nor is alb on this gas
And form a mixed NAGMA/HAGMA no less...more than one cook
What could be causing the NAGMA?
- Renal > Renal Tubular Acidosis? CAI? No electrolyte patterns to suggest or drug history (acetazolamide etc)
- Lower GIT? No symptoms
- HHS? Maybe, but glucose isnt as high as you would traditionally think
- Extra Cl-? (Cl okay)
- Recovering DKA? Well...we havnt started any treatment
What could be causing the HAGMA?
- Ketoacidosis? Ketones 8.0 mmol/L, so yes!
- Lactic Acidosis? 1.6 mmol/L, so no
- Renal Failure? Crea 68, so no
The interesting thing about this patient, is that they he is on dapagliflozin.
"What's that again?" I hear you ask? Its an SGLT2 inhibitor antihyperglycaemic.
Why is this important?
Theres growing evidence that suggests that SGLT-2 inhibitors directly cause euglycaemic diabetic ketoacidosis
ie they're very sick and need emergent resuscitation - so just because someone looks like they're in DKA but have an okay-ish BSL, dont think its not...
So whats the management?
Largely the same principles as DKA
- Fluid resus ensuring you keep an eye on blood glucose, chlorine, potassium and pH
- Insulin to close the anion gap and reverse the metabolic acidosis
- Will probably need IV dextrose given starting BSL (before insulin is given) is already not that high
- Note that for this patient, insulin may improve the metabolic acidosis fast enough and the patient may need more rapid correction of acidosis with NaHCO3 or haemofiltration
So what precipitates eDKA?
- Carbohydrate restrictions
- Fasting
- Dehydration
- Alcohol
- Partially treated hyperglycaemic DKA
Nerding Out: How do SGLT-2 Inhibitors cause euDKA?
- SGLT-2-I decrease serum glucose
- reduced serum glucose reduces insulin > increases lipolysis > increases free fatty acids
- reduced serum glucose also increases glucagon > reduces acetyl-CoA Carboxylase > increases carnitine palmitoyltransferase-I
- Both mechanisms > increases B-oxidation > causes ketone production > euDKA


 RSS Feed
RSS Feed
